Published September 30, 2022

Avneesh Chhabra, MD, MBA
@AChhabraMD
Professor of Radiology
Chief of Musculoskeletal Imaging
UT Southwestern Medical Center
Parkland Health & Hospital System
Collectively, ultrasound, electromyography, and even physical findings play a role in diagnosing anomalies of the peripheral nervous system. Increasingly, though, MR neurography (MRN) is becoming very common for the evaluation of peripheral neuropathy. This enhanced adoption is due to technological advancements in imaging quality and acquisition speed, such as newer 3D techniques, improved coil equipment, sparser k-space sampling, and compressed sensing, etc. In fact, in today’s tertiary care setups, MRN is being quickly incorporated for the workups of peripheral neuropathy and plexopathy patients, due to both need and ask from the peripheral nerve physicians, orthopedic surgeons, and pain management specialists. Although many articles about the evolution of MRN have been published in the clinical literature, thus far, no standards for the evaluation and recording of peripheral nerve pathologies on MRI have been acknowledged, much less validated.
NS-RADS Debuts in AJR
Until the August issue of AJR, that is. In “Neuropathy Score Reporting and Data System (NS-RADS): A Reporting Guideline for MRI of Peripheral Neuropathy With a Multicenter Validation Study,” my colleagues and I proposed a standardized classification for evaluating and reporting peripheral neuropathies. Accurate and reliable across different reader experience levels and a spectrum of peripheral neuropathy conditions, NS-RADS also improves multidisciplinary communication.
Our retrospective study included 100 patients with nerve imaging examinations and a variety of known clinical diagnoses. Utilizing mutually agreed-upon qualitative benchmarks for classifying and grading peripheral neuropathies, different classes were established to account for the spectrum of underlying pathologies (unremarkable, injury, neoplasia, entrapment, diffuse neuropathy, not otherwise specified, and postintervention state) with subclasses to describe lesion severity or extent. Validation was performed by 11 fellowship-trained musculoskeletal radiologists across 10 institutions, and after initial multimedia training, all 100 cases were blind-presented to readers (Fig. 1).


Offering a uniform lexicon and practical guideline for reporting neuropathic conditions on MRI, ultimately, NS-RADS accuracy for determining milder versus more severe categories per radiologist ranged from 88% to 97% for nerve lesions and from 86% to 94% for muscle abnormalities (Fig. 2).


On the basis of the overall promising interrater agreement shown in this study, we believe that the newly proposed NS-RADS classification will perform as well in routine practice as it did in this initial validation study (Fig. 3).


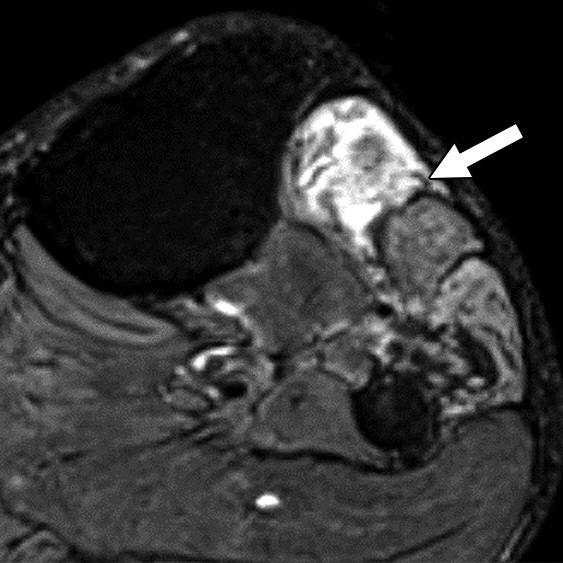
Axial (left) and oblique coronal (right) fat-suppressed T2-weighted images show proximally enlarged and hyperintense ulnar nerve (arrows) and normal nerve caliber distal to cubital tunnel (arrowhead on right).
However, we must acknowledge several barriers that still exist for learning and successful incorporation of routine MRN in radiology practices:
- lack of widespread usage of technology, especially information on recent advancements
- optimization for different tissue resolutions
- complexity of peripheral nerve anatomy
- uniformity of reporting with multidisciplinary teams
- paucity of knowledge about diagnostic imaging criteria for lesion classification—something NS-RADS intends to correct
NS-RADS Details at ARRS Annual Meeting in Hawaii
Presented live during the 2023 ARRS Annual Meeting in Honolulu, HI, “MR Neurography and NS-RADS: Assist Your Neuropathy and Pain Patients” will focus on the latest advances in MRN and its practical application in routine imaging practice. Pertinent for practicing radiologists, musculoskeletal and neuroradiology subspecialists, fellows and residents in diagnostic radiology, and even radiologic technologists, six experts in MRI protocol and sequence design will deliver a two-hour categorical session. This session has been expertly curated, covering one anatomic site at a time. The majority of our lectures will be nerve-focused—reviewing and updating NS-RADS and detailing innovative MRN techniques for brachial plexus, LS plexus, facial, intercostal, as well as peripheral nerves. Our panel will also address 2D vs. 3D MRI correlations, highlighting relative advantages and disadvantages of different sequences.
Moving forward, modern MRI readers need to be fluent in the latest MRN features of different neuropathies, as well as related syndromes and classifications. We will also discuss current research projects and future applications. By incorporating these imaging interpretation criteria and expert insights from different tertiary care institutes, imaging professionals can impact diagnostic strategies, thus altering management decisions of neuropathy patients for improved outcomes.
The opinions expressed in InPractice magazine are those of the author(s); they do not necessarily reflect the viewpoint or position of the editors, reviewers, or publisher.